Gluteal tendinopathy: You don't need orthopaedic or nhs, try this instead.
Feeling a twinge in your butt?
Picture this.
You stay in shape, jog, and visit the gym but one morning you wake up with discomfort on the side of your butt.
You take a break, and it improves but when you return to the gym it resurfaces once more.
Even small things that you usually find easy cause pain.
So what could be happening?
You might be dealing with gluteal tendinopathy, also known as gluteal tendonitis. Basically, it's when the tendons in your arse muscles get irritated or inflamed.
Give this a try - if you stand up straight and feel around the side of your hip, you'll find a bony spot called the greater trochanter. That's where the gluteus medius and gluteus minimus tendons attach, right on your thigh bone.
If this is sore then you could have pain from gluteal tendinopathy or otherwise known as greater trochanteric pain syndrome.
https://e3rehab.com/
https://e3rehab.com/
These tendons are like the bouncers of your hip joint, helping you stand tall, walk, run, and climb stairs without tipping over.
But when they get overworked from activities like running, stair-climbing, or even sitting down for too long, they can start acting up. And boy, does it hurt.
You might feel some achiness and pain in your hip, pelvis and butt area.
There is also a trochanteric bursa in the same area, which is a fluid-filled sac that serves to cushion and reduce friction in this area. Over the top of these structures lies the Iliotibial (IT) Band.
Getting the right diagnosis is important but when it comes to treatment, most of the treatments are similar and the majority of the treatment should be exercise rehabilitation.
In the form of a graded strengthening program which is likely to take 8-12 weeks of hard graft.
If you keep reading, I will give you a step-by-step rehab plan and physical therapy treatment can help you overcome to overcome lateral hip pain and also how to return to running, sports or the gym quickly.
gtps - https://www.upsidehealth.com.au/blog/pain-profile-gluteal-tendinopathy
What causes gluteal tendinopathy/lateral hip pain?
So, you went to the doc and got the news that you've got gluteal tendinopathy. It's like an alien term to you, so naturally, you turn to the all-knowing Dr. Google for some answers.
Next thing you know, in just 5 minutes, you're convinced that you need some kind of invasive procedure or surgery.
You read horror stories of it going on for years and people having to give up sport and exercise but before you let your mind wander.
Wait a minute, is this the only option? Surely, there is another way? I can reassure you that there is so keep reading to find out more.
So what if you got diagnosed with trochanteric bursitis? is the treatment any different?
Forget about blaming your hip pain on bursitis, research from the past 20 years (Bird et al 2001, Connell et al 2003, Kong et al 2007, Silva et al 2008, Blankenbaker et al 2008, Woodley et al 2008, Fearon et al 2010, Long et al 2013, Lange et al 2022) has shown that it's probably not the real culprit.
In fact, MRIs often catch bursitis in hips that aren't causing any pain at all. For instance, a study by Woodley et al in 2008 found that bursitis was "equally prevalent in symptomatic and asymptomatic hips." So, having bursitis in both hips but only feeling pain on one side is normal.
Much of the same research found that the tendons of the gluteus medius and minimus are more often involved which explains that 9/10 is gluteal tendonitis and not bursitis.
https://www.running-physio.com/
How to test whether you have it?
Most people will present with pain on the outside of their hips when walking and climbing stairs but in addition, Grimaldi et al in 2017 concluded that “…a patient who reports lateral hip pain within 30 seconds of single-leg-standing is very likely to have gluteal tendinopathy.”
If you have concerns that its something else e.g. hip osteoarthritis or low back-related issues then get an appointment with either your GP, a local sports Physiotherapist or give me an email via hello@functionalmovementphysio.co.uk or reach out on social media to discuss this.
As long as hip osteoarthritis, low back-related issues, and other similar conditions have been ruled out, simply calling it lateral hip pain is a good option. So many of my clients get lost in "analysis paralysis" due to over-diagnosis and never commit to an evidence-based treatment plan.
What causes gluteal tendinopathy or lateral hip pain?
Well to put it simply, it's often from "doing too much, too quickly" without giving your body enough time to get used or recover from the new stress/ load you have put through your body.
Running example
I had a lady recently training for the London Marathon. She had a rest over Christmas but then suddenly increased her mileage to 5 runs per week with a combination of speed work and long distance.
One week in she developed pain on both sides of her hips. On assessment, she had weak glutes/hamstrings and pain in pressing her glute muscles. She could not understand why this had happened to her and was frustrated because of it affecting her training for the London marathon.
She kept training for a week but got to the point where she was in pain when sleeping at night and struggling to walk/run in the mornings. She was scared that I was going to tell her to "STOP RUNNING", the dreaded words no runner wants to hear. But I didn't, we lowered her training whilst working on reducing her aggravating factors and increasing her strength. She's not back running and looking forward to her first London Marathon.
This is not always possible but with the right treatment you have a better chance than secretly going to bed and waking up in the morning hoping your pain magically vanished.
https://e3rehab.com/
CrossFit example
I had a chap who had been fairly inactive for years due to a busy office job until one day he had a heart episode and wanted to change his health.
His best friend invited him to a CrossFit gym. He fell in love with and started to increase his training. He was invited to compete in a CrossFit competition so upped his training considerably including squats, deadlifts, snatches etc.
On one day in the gym during his weighted squats he felt a pain in his left glute, he ignored it and trained through it. It gradually got worse until he got pain doing everything things like walking, bending, stairs etc. Then he came into the clinic.
So what does this all mean?
Look at the picture below.
https://e3rehab.com/
When the load through your muscles, joint and tendons outweighs the capacity for your body to adapt and recover then gluteal tendinopathy may develop.
Increased load can be in many forms...
More weight
More sets
Less rest during sets
More training days
New exercises/activities
Less rest days
More sitting down/ standing long periods
Poor sleep
Poor nutrition
Stress
Alcohol/drugs
Calorie deficit
Change in metabolism
Diabetes
High cholesterol
Obesity, and certain medications like statins and antibiotics, also impact the health of the tendons.
Any of these changes can make a HUGE difference. People often feel like they've not changed anything but when I dig into their history, something always has changed. That's the detective work you get from a sports physiotherapist.
Who is most commonly affected by Gluteal Tendinopathy?
The research indicates that it is more prevalent in women. One specific group of women who are affected by this condition are those who engage in running.
The repetitive strain on the gluteal muscles and tendons during running can lead to gluteal tendinopathy if the frequency, volume, and/or intensity of the runs exceed the body's ability to recover and adapt properly.
However, gluteal tendinopathy more commonly affects older, less active perimenopausal women. While loading of the gluteal tendons plays a role in the development of this condition, it has been well-documented that other factors related to lifestyle and metabolism, such as diabetes, high cholesterol, obesity, and certain medications like statins and antibiotics, also impact the health of the tendons.
Gluteal tendinopathy is complex and multifactorial. It’s useful to acknowledge the role of tendon loading in its presentation, but the importance of your overall health and well-being cannot be overlooked.
Thankfully, either way, there are a lot of management options so let's talk about them so you can get back to the things that you love ASAP.
Stage 1 - Activity Modification/Lifestyle change
Skipping this step is a big no-no.
It's crucial to tweak the load and reduce the things you do that aggravate your symptoms if you want to succeed long term.
And I want to make this clear.
Most people do not have to stop doing what they love completely.
But usually, it means reducing some load temporarily whilst you improve your tissue capacity (or the ability of your tendons to tolerate the load).
Picture this: you get smacked in the face, and then every day you smack yourself in the face again.
What do you think would happen? Yup, your poor face would never get a chance to heal and it would just stay sore. Ouch!
These are some activities that you should think about changing as they have been shown to have an impact on long-term gluteal pain.
Sleeping position - this can cause compression and symptoms of gluteal tendinopathy.
On back with a pillow under knees
https://casper.com/blog
On side with pillow between knees - Having a pillow between knees can reduce compression of your glutes overnight.
https://casper.com/blog
Sitting posture: Spending extended periods sitting down - If you experience discomfort while seated, you may want to see if the pain worsens when you cross your legs, sit in a low or deep chair, or remain seated for an extended period.
https://e3rehab.com/
Stairs - If you experience discomfort while using stairs, be sure to utilise the handrail on the opposite side of your painful hip whenever possible. If this is still challenging, ascend the stairs one step at a time with your non-painful side leading.
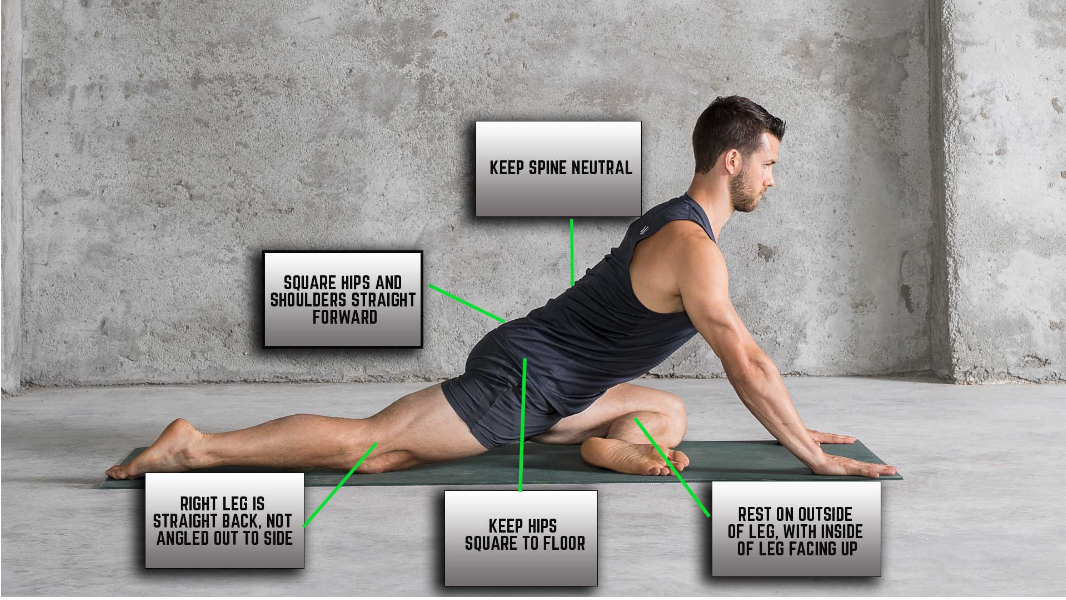
Stretching - Engaging in end-range stretches, which are often recommended by other healthcare professionals for this issue, has been proven to exacerbate symptoms of lateral hip pain. Therefore, please avoid doing exercises like the pigeon pose.
https://manflowyoga.com/blog
Walking/ running - If you experience discomfort while walking or running, it is important to adjust how often, how much, and/or how hard you run to find a level that you can handle without flaring up your pain or symptoms. As a rule, you're pain should be no more than a 5/10 during or after exercise.
Running cadence - You can also try increasing your running speed (cadence), which is the number of steps you take in a minute, by 5-10% to reduce strain on your buttocks. To do this download the Run Cadence app, it's free on the app store. Work out what cadence you run at naturally then add on 5-10%. Its super easy and the app will help you with this.
https://e3rehab.com/
Understanding what's aggravating you in the first place is the hardest thing and the most difficult thing to admit.
That's why working with a sports physiotherapist can make a big difference as they can look at your life from a holistic viewpoint and make recommendations accordingly.
Also don't forget the other areas previously mentioned...
Poor sleep
Poor nutrition
Stress
Alcohol/drugs
Calorie deficit
Change in metabolism
Diabetes
High cholesterol
Obesity
Medications like statins and antibiotics.
This is when speaking to a doctor or a health coach to complete a physical examination can help you tackle some of these whilst you introduce strengthening into your program. Being honest with yourself r.e. weight gain etc can be difficult but will help you reach your goal.
Understanding Gluteal Tendon Rehabilitation
This is a step-by-step approach to how to strengthen the muscles you need to reduce your gluteal pain. It is based on evidence but the pictures are taken from E3 R3hab.
Stage 1 - Best Exercises for Gluteal Tendinopathy
https://e3rehab.com/
https://e3rehab.com/
https://e3rehab.com/
https://e3rehab.com/
https://e3rehab.com/
Phase 3 - Advanced Strengthening Exercises
https://e3rehab.com/
https://e3rehab.com/
https://e3rehab.com/
https://e3rehab.com/
Stage 3 - Plyometrics and return to sport
This stage is specific to your sport and activity. Once you get to a level where you are pain-free during the exercises above going straight back into your sport/activity too soon without a plan is a nightmare waiting to happen. Seeking help from a specialist physiotherapist at this point can make a massive difference.
Feel free to give me a message and we can organise 1-2 sessions of face-to-face or virtual physiotherapy so that you are doing the right things at this stage.
Going back too early without stage 3 done correctly can take you back to stage 1 if not done strategically and gradually based on load/pain.
Shoot me a message/email at hello@functionalmovementphysio.co.uk and we can arrange a free 30-minute call to make sure that you are doing everything you should to become pain-free from gluteal tendinopathy.
Pain monitoring and symptom management
And although tracking your pain intensity can be useful in certain situations, don’t only tie your successes or failures to its fluctuations. Consider answering other questions throughout the rehab process to reflect on your progress. For example:
Do you have more control over your symptoms?
Are you exercising more regularly?
Has your function improved?
Are you sleeping better or walking more?
Are you doing more of the things you enjoy?
Let me put all of this information together by presenting 2 case examples.
https://e3rehab.com/
Orthopaedic Approaches to Managing Gluteal Tendinopathy Pain
Since these “pathological” findings are present in individuals with and without symptoms, imaging is unnecessary in most instances.
Sometimes an MRI is used to confirm a hypothesis but should not be the first option as it can show red herrings that aren't causing pain.
People who head down the MRI pathway too so often end up with steroid injections and sometimes surgery that they do need.
Even if you have injections or surgery you still need to build up your capacity and strength with exercises so why don’t you start there rather than having something that you don’t need?
To summarise what we’ve just discussed
Summary
Most lateral hip pain is Gluteal tendinopathy or pain on the outside of your hip.
It’s unlikely to be bursitis according to research spanning 20 years.
It is characterised by moderate to severe pain with activities that load the gluteus medius and minimus, such as standing on a single leg, walking, running, and going upstairs, as well as sleeping on the affected side.
The diagnosis is most common in older, less active women, but it can also occur in runners.
Although some individuals will get better with time, a primary focus of management should include modifying any aggravating activities and specific musculoskeletal exercises can be performed to improve the conditioning and function of the glute muscles.
Having a thorough biomechanical assessment by a sports physiotherapist is essential to target it with the right corrective exercises but if you don’t want to then the exercises in the blog are a great place to start. The most difficult thing to judge is getting the load right.
TOO MUCH TOO QUICKLY = PAIN
TOO LITTLE = NO IMPROVEMENT
JUST RIGHT = RELIEF
Since gluteal tendinopathy may be associated with other health-related issues such as diabetes and hypercholesterolemia, any lifestyle interventions to improve overall health (like regular physical activity) should be considered.
Regardless of what you decide to do, it’s important to tailor the plan to your individual goals and needs.
There is no quick fix for gluteal tendinopathy, so it’s helpful to set realistic expectations and plan for the process to take a minimum of 3 months.
If you want to be added to my email list for more hints, tips and special offers, follow the link below
Much Love,
Stuart Goldfinch (Specialist Sports Physio, Running Expert, Ex UK SAS Trainer, Head Physio Merseyside Police)
P.s. Please feel free to reach out for advice, a moan or just to say hey! I’m here to help you achieve your goals.